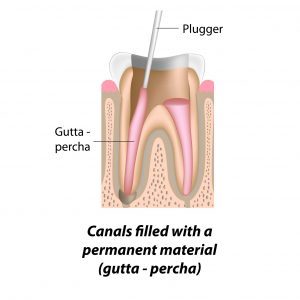
Second Stage: Filling Of The Canal /Canals
After cleaning and drying, it will be time to fill each root with a sealer paste and rubber material. The tooth will be restored with a filling material on that visit.
Cracked tooth syndrome occurs when a tooth has a crack that is too small to show 
Root canal treatments at the Surbiton Smile Centre ® is a dental procedure used to treat infection in the root canal system. It is a treatment to repair and save a badly damaged or infected tooth instead of removing it. The term ‘root canal’ refers to the canals inside the root of the tooth.
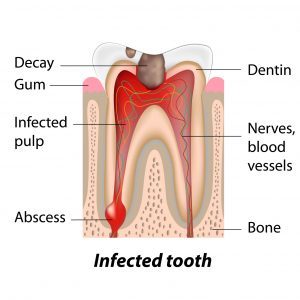
The pulp extends from the crown — the visible part of the tooth — to the tip of the tooth’s root in the jawbone. The pulp contains nerves, blood vessels and connective tissue.
A single tooth can have more than one root canal and Molar teeth in particular have several roots. When a tooth is cracked or has a deep cavity, or if there is a leaking filling or perhaps the tooth is damaged as a result of a trauma like an accident or fall, bacteria can enter the pulp.

If it is left untreated, bacteria and decaying material can cause a serious infection or a tooth abscess, leading to pulp death, bone loss or loss of the tooth itself. Signs and symptoms may include swelling around your face and neck, a hole in your tooth, toothache /tooth pain, gum swelling, temperature sensitivity, headaches, pain when biting or chewing, swelling of the gum near the affected tooth, pus oozing from the affected tooth, facial swelling and the tooth becoming a darker colour.
It is important to see our Dentist if you have a problem with your tooth as soon as possible in order to avoid possible nerve damage and thus avoid root canal treatment.
To treat the infection in the tooth canal, the bacteria existing there needs to be removed. This can be done in following way ;
Using a dental tool that is shaped like a long slim round file the bacteria is removed. The root canal is then filled, and the tooth is sealed with a filling and a crown. In most cases the inflamed tissue around the tooth will heal naturally.
Root canal treatment usually takes two visits, but sometimes additional visit are required as some teeth may prove difficult to treat. First, you will a have dental X-ray to check the extent of the damage. You will also receive a local anaesthetic to control the pain. This pain can be more severe if the tooth has developed an abscess. Then a rubber sheet (called a rubber dam) is placed around the tooth to keep the tooth clean and free from saliva. The tooth decay is removed, and an opening is made through the crown of the tooth to gain access to the pulp chamber. Using a small dental instrument, the infected or diseased pulp is removed.
During the procedure our dentist will use a series of root canal files to reshape the canals. The root canals will be flushed and cleaned with antiseptic liquid several times during the treatment. Where applicable each canal will be enlarged to allow better access for cleaning and flushing and the filling in of the canals at a later stage.
This part of the treatment may take several hours to complete, and it may need to be carried out in several visits. If this is the case, a dressing (medication) will be placed inside the cleaned canal to kill the infection and the tooth will be provided with a temporary filling.
In severe cases, where the infection has spread behind the tooth and you have a large swelling which is fluctuating, the tooth may be left open in order to allow the infection to drain away, normally for a period of 24 hours.
Our Dentist will prescribe you an antibiotic when you have a fever, large swelling and severe pain due to the infection. The premolar teeth and the back molar have between 2-4 roots and each root has 1-2 canals. The teeth in the front and the cainan have one root and one canal. The more canals a tooth has, the longer the time becomes to treat the tooth.


After cleaning and drying, it will be time to fill each root with a sealer paste and rubber material. The tooth will be restored with a filling material on that visit.
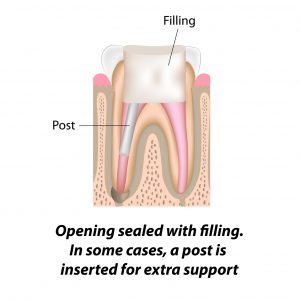
The root filled teeth are more fragile after root canal treatment and need to be protected from future damage in the form of a fracture. Our Dentist will normally recommend you have it crowned as soon as possible. If the tooth fractures, it will make it impossible to save the tooth again.
If the remaining tooth structures are not enough to support a crown, the tooth must be built up with a small metal post prior the crown treatment.
The crown is a cap which will covers the tooth. To be able to fit the crown the tooth will be made smaller and re-shaped. A mould will be taken to have the crown made to fit over the tooth.
The crown can be made from the following materials:
After root canal treatment you will be advised to follow good dental and oral hygiene, in order to ensure that your restored tooth lasts a long time. If you experience pain in the first few days after root canal treatment, you can take painkillers, but if the pain or pressure lasts a few days, then please make sure you contact the Surbiton Smile Centre ® immediately.

Even though endodontic treatment is one of the most successful and predictable procedures in modern dentistry, failures can occur. Some indications of failure include swelling, soreness or the persistence of abscess at the root tip as identified in an X-ray. When this happens, a root canal revision procedure, also referred to as “re-treatment,” may be warranted.
Although retreatment is technically more difficult than the original root canal, it can usually rescue a failing condition without having to consider surgery. We at Surbiton Dentist especially well equipped to handle these difficult conditions because of our additional training and experience.
Conventional root canal treatment is not always sufficient to correct every patient’s condition. Occasionally, endodontic surgery is required. This is because a previous treatment has deteriorated or because anatomic considerations such as the shape of the tooth or canal space make the traditional root canal treatment especially difficult to complete.
If you experience sensitivity following a root canal session, we recommend you take an anti-inflammatory drug such as ibuprofen to reduce inflammation, which will in turn reduce pain. You may also want to apply ice to the outside of your face next to the tooth, keeping the head elevated.
Under no circumstances should you apply heat to the outside of your face. Consistent medication is the key to comfort. It is essential to follow your dentist orders by taking prescribed medications to alleviate pain and to help prevent or fight infection. If discomfort lasts more than a few days or if you have severe pain or swelling, call our office. We will suggest medication or other steps to make you more comfortable
Sometimes Root Canal Treatment can be completed in just one visit, but normally it takes two or three appointments depending on the individual tooth anatomy and other circumstances.
Quite often this treatment is needed to relieve the existing pain that already exists. With modern techniques and the use of local anaesthetic, the procedure is pain free. If the tooth has a severe infection, it may take longer for the tooth and gum to become numb. In such a case our Dentist will inject further local anaesthetic.
It is possible that you may feel some discomfort afterwards. Taking normal painkillers will usually soothe the pain. If this does not do the trick, and the pain persists, you should contact us as soon as possible.
The cost of Root Canal Treatment varies and is dependent on how severe the underlying problem is. For example, the molars have three to four canals and are therefore more difficult to treat. If you have a tooth with a severe abscess, then several visits might be required to achieve a good result. Factors such as these will increase the root canal cost.
There is only one alternative to this type of treatment and that is an extraction. Unfortunately, not all damaged teeth can be repaired (restored) and hence an extraction is sometimes necessary. The resulting missing gap is then filled by a removable denture, a fixed dental bridge or a dental implant.
This procedure has a high success rate, as long as it is performed to a high standard. At the Surbiton Smile Centre ®, we will ensure that this is the case. But occasionally no matter how high the standard of care is, the root filled tooth never heals up, which will result in the loss of that tooth. Also, Root Canal Treatments can fail if the tooth develops further decay, or the existing restoration fails resulting in leakage, or the tooth suffers later from a crack or fracture. A further possibility maybe due to the difficult anatomy of the tooth which made it difficult to clean the narrow and curved canals to eliminate the bacteria entirely.
You must visit us at least once a year to make sure the tooth is healing up. This really should be part of your regular six-monthly visits that form part of your routine check-ups.
Root canal treated teeth can last for a long time but sometimes the treatment fails, or the patient’s symptoms persist. This can happen immediately after the completion of the root canal treatment, but if it does happen then quite often it is much later.In such an instance, the treatment must be performed again, and that procedure called root canal retreatment.
All our Dentists at the Surbiton Smile Centre ® can carry out this procedure. Obviously, retreatment is more complicated and time-consuming and may require the use of a microscope.
A tooth fracture can be responsible for pulp exposure resulting in the injury or demise of the pulp.
A careful and complete diagnosis must be made on each and every suspected tooth.
The sequence of endodontic problems diagnosis is as follows:
Medical history:
Patient with pace maker: Dentist must refrain from a procedure that would interfere with pacemaker function: e.g. pulp testing sonic devices like apex locator, electro surgery etc.
Dental history:
Purpose: Quite often the problem tooth can be localised by taking the dental history.
The following are typical question that may be asked:
Purpose: Careful questioning of the patient must be conducted to evaluate the patient’s problem completely. A tentative diagnosis can often be made from these subjective symptoms.
These are the objective signs observed by the dentist in an around the mouth. It is important to note the following:
Purpose: Often problematic teeth can be localised, and the dentist may see other contributing factors involved. Judgement is made on whether the involved tooth is worth salvaging.
These tests are mandatory to confirm any tentative diagnosis that has been made so far. All eight of these tests must be used and in certain case further selective tests must be used:
Outside of root:
Inside of root:
Purpose: The status of pulp and periapical tissue can be evaluated, and diagnosis can be confirmed.
The cracked tooth syndrome refers to a crack within the crown of the tooth without any pulpal involvement.
It usually manifests itself as sensitivity to a certain biting pressure. It becomes very painful when biting in one direction. Also,an extreme reaction to cold sets it off.
A different diagnosis must be made between sinusitis, nerve pain, overloading contact, grinding problem, or TMJ problems.
Any large amalgam filling which does not protect the cusp should be suspected.
The older the patient or the greater the intercuspation and wear, the greater the possibility of a crack.
One should always think of a cracked tooth when all other tests prove negative.
Differential diagnosis of anatomical land marks or pathological lesion from inflammation around the root
Following procedures required:
up in an X-ray or is under the gum and therefore challenging to identify. It most often appears on molars.
A crack in your tooth can be hard to detect simply because these fractures are often invisible to the human eye. In fact, hairline cracks may not even appear on X-rays. So how can you tell if your tooth is fractured? Look out for localized pain that flares up when you bite into food or when you expose your teeth to hot or cold temperatures. The pain or discomfort will not be constant, as with a cavity.
Several behaviours and incidents can lead to a crack, also known as a fracture, in one of your teeth. In some cases, simply chewing on a hard object or type of food such a biscuit or ice can cause a crack to develop. Habits that are sometimes related to stress, including tooth grinding or jaw clenching, can also make your teeth more susceptible to fractures. Occasionally, an accident or forceful trauma may lead to a cracked tooth.
At the Surbiton Smile Centre ® our Dental team will recommend the best treatment depending on the severity and location of the tooth fracture. Treatment options include:
Tooth sensitivity occurs when the enamel that protects your teeth gets thinner, or when gum recession occurs, exposing the underlying surface, the dentin, thus, reducing the protection the enamel and gums provide to the tooth and root.
If hot, cold, sweet or very acidic foods and drinks, or breathing in cold air, makes your teeth or a tooth sensitive or painful, then you may have sensitive teeth. Tooth sensitivity can come and go over time.
See your dentist at the Surbiton Smile Centre ® to check your teeth for a cavity, cracked tooth, misalignment, or gum disease
 Dr. Simin Soltani (Principal dentist)
DDS . MSC . Sweden
Dr. Simin Soltani (Principal dentist)
DDS . MSC . Sweden
 Dr Shima Mahdavi-Izadi
DDS, MClinDent MEndo, Specialist Endodontist
Dr Shima Mahdavi-Izadi
DDS, MClinDent MEndo, Specialist Endodontist
Please get in touch if you are concerned about any aspect of your dental health. We will treat you fairly and honestly - and we look forward to being able to help you.
