Overview

Periodontal treatment or gum disease treatment at Surbiton Smile Centre ® involves thorough diagnosis and comprehensive treatment of the single largest cause of tooth loss in older people. There are several types of periodontal disease, and all of them are caused by bacterial infections, which attack the gums, jawbone and the ligaments that hold the teeth in the jaw. Periodontal disease usually starts silently, painlessly and without any significant symptoms. It can make slow or rapid progress depending on its severity.
What Is Periodontology?
Periodontology is the specialised study of hard and soft tissues that supports your teeth and maintains position in the jaw. The periodontium, which are the specialised tissues support the teeth and have two important functions: firstly,to securely attach the teeth to the jaws; this acts as an impact absorber during biting and chewing helping to prevent tooth damage; secondly it maintains the teeth in a stable position within the jaws so that they work efficiently and comfortably during chewing.
The periodontium is made of several component structures that work together. The tooth socket is the bony pouch in the upper or lower jawbone where the tooth is positioned. Below the gums, the supporting root/roots of the teeth. These roots are not usually visible in a healthy mouth and extend into the tooth socket, covered by a layer of cementum. Extending between the root, cementum and the socket are a complex arrangement of tiny fibres known as the periodontal ligament, which holds the tooth in place almost like a sling. Because the different parts of the periodontium are made from living tissues, they can adapt to changes in our mouths over time, making tiny changes in shape and thickness that keep the teeth stable.
Why Is Periodontology Important?
Often the mouth can reflect the condition of your body. In particular, the periodontal status can divulge more than what is simply happening in the gums. Although periodontitis is always triggered by plaque accumulation on the teeth, diseases affecting the rest of the body, known as systemic diseases, can weaken the supporting structures of the teeth.
In certain cases, some serious disorders are known to reveal symptoms in the mouth before they are evident in any other part of the body. Therefore, often a trained periodontist is the first person to detect the signs of general disease, such as diabetes or blood disorders during an oral examination. Because the association with general health overlaps with other medical disciplines, periodontology can rightly be regarded as a ‘holistic’ form of dentistry.
What Is Periodontitis?
Periodontitis, commonly referred as ‘Gum Disease’, is a common condition which the gums and deeper periodontal structures become inflamed. This inflammation usually takes the form of redness, swelling and tendency to bleed during brushing. This is the body’s response to certain bacteria that have been allowed to accumulate on the teeth. Although this is part of the body’s defence system, the inflammatory response can eventually cause serious damage. If left unchecked, the inflammation can spread down below the gums and along the roots of the teeth, causing destruction of the periodontal ligament and supporting bone. This ultimately leads to the loosening and potential loss of the teeth.
Periodontitis is the leading cause of tooth loss.
How Can I Recognise Periodontitis?
Early Periodontal Disease
Periodontitis is caused by certain bacteria (known as periodontal bacteria) and by the local inflammation triggered by those bacteria. Although these bacteria are naturally present in the mouth, they only become harmful when conditions are right for them to dramatically multiply. This happens when a layer of bacteria and food debris, known as plaque, builds up and is left undisturbed on the teeth, commonly in hard-to-reach areas such as between the teeth.
Other more dangerous bacteria can thrive, producing some harmful by-products which then stimulate the body’s defensive inflammatory response in the gums. As the disease progresses, chronic inflammation causes the bone of the jaw to be destroyed and the teeth to be lost. In many people, this is a gradual process that takes place over many years and, if detected and treated, can be halted. However, some adults have a very aggressive form of the disease which causes early loosening and loss of the teeth.


Advanced Periodontal Disease
Periodontitis starts with inflammation of the gums, known as gingivitis. This is not always easy to recognise but one of the first signs that you may become aware of is bleeding from the gums when brushing your teeth. The gums may appear red and swollen and possibly notice a discoloured layer of bacterial plaque on the teeth.
If left untreated, gingivitis may progress to periodontitis, often without any obvious signs to alert you. However, some changes you might experience over time include:
- increased bleeding from the gums; which may be provoked by brushing, eating, or even be spontaneous
- bad breath
- changes in the positioning of the teeth in the jaws
- lengthening of the teeth (gum recession)
- possible pain.
Bleeding from the gums may be less noticeable in smokers, because of the effect nicotine has on blood vessels, and so the disease process may be masked.



More Advanced Inflammation
The presence of periodontitis is not often recognised by an individual until they are 40 or 50 years of age, by which time a great deal of damage may have occurred. However, a dentist can detect signs of the disease at a much earlier stage during a routine examination and can monitor your periodontal status using a special assessment known as the Periodontal Screening Index.


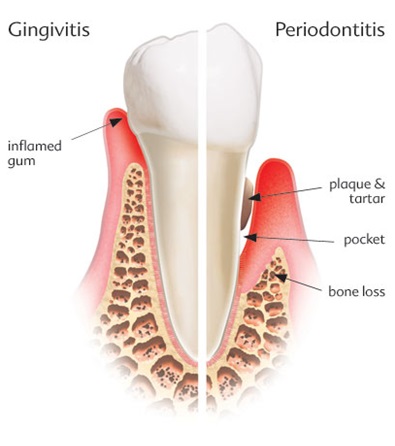
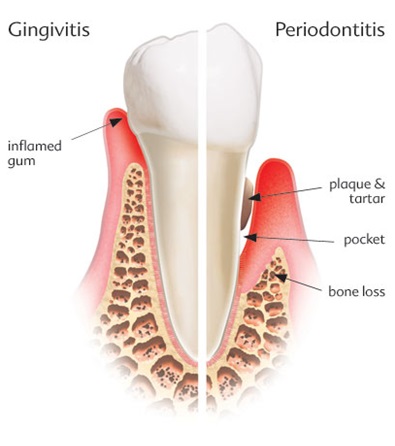
The Process Of Gum Disease Development Can Be Demonstrated By The Schematic Pictures Below:

Periodontitis can be understood better when we have an idea of the anatomy of the tooth and its supporting structure.
In almost all cases, periodontitis starts with gingivitis.

In susceptible patients, plaque and tartar will cause irritation of the gums and bone loss. This condition is called periodontitis.

Bone loss means that the support of the tooth is reduced. Uncontrolled bone loss leads to tooth loss.

When periodontitis is present:
- Pocket depth increases due to swelling and bone loss.
- The gums may bleed more easily when touched.
- The supporting bone level is reduced around the tooth.Uncontrolled periodontal disease is a common cause of tooth loss in the adult population.
What Are The Causes Of Periodontitis?
A healthy mouth is colonised by more than 700 different species of bacteria, most of which are completely harmless and live in harmony with their host. However, when tooth cleaning is not thorough enough, bacterial deposits build up next to the gums, forming a soft plaque, and the conditions become suitable for more dangerous bacteria to flourish. The natural defences of the body are also compromised.
In all cases, periodontitis is caused by the build-up of bacteria in the form of dental plaque.
If the soft bacterial plaque is not removed by brushing, minerals are deposited within it over time and it becomes a hard deposit on the tooth called tartar. The presence of tartar encourages further growth of the bacterial plaque towards the roots. As the inflammation progresses deeper, the attachment of the gum to the root is disrupted and a gap or periodontal pocket is formed. This is an ideal place for harmful bacteria to colonise and multiply, accelerating the disease process. In their new habitat, the bacteria release toxins as by-products of their metabolism, which further trigger the body’s defence mechanisms.
The severity and progression of periodontitis depends upon the balance of several factors: the number and type of bacteria present, how strong the individual’s defence mechanisms are, and the presence or absence of certain risk factors. For example, the more aggressive the bacteria and the weaker the immune response of the patient, the more active the disease will be. Added to that, some risk factors, such as smoking or diabetes, can further weaken the body’s defences and accelerate the disease process. In the same way, certain drugs, such as antihypertensive or vasodilating agents and immunotherapy, affect inflammatory responses to plaque and patients more susceptible to gingivitis. However, it is important to recognise that, without the accumulation of bacterial plaque, periodontitis will not occur.
What Can I Do To Prevent Periodontal Disease?
Periodontal inflammation is not inevitable. The development of gingivitis and periodontitis can be prevented by adopting thorough oral hygiene habits, alongside regular professional examinations and support.
The basic elements of a good oral hygiene regime are:
- Cleaning the chewing surfaces and sides of the teeth twice daily, with a toothbrush (of appropriate size and good condition) and toothpaste
- Cleaning the spaces between the teeth where the toothbrush bristles cannot reach, by using either dental floss or an interdental brush, depending on the size of the space. This should be done once daily.
While interdental brushes are suitable for larger gaps, dental floss should be used where teeth are close together, with little or no space between them. Special care should be taken to thoroughly clean around crooked or crowded teeth, around fillings, crowns and dentures as plaque accumulates readily in these places.
Antibacterial mouthwashes are a useful supplement to brushing, which inhibit bacterial growth and dampen inflammatory changes. They should be used after tooth brushing.
If, as a result of an inadequate cleaning technique, plaque deposits are left on the teeth, these will become mineralised and turn into hard, fixed deposits (calculus, commonly known as tartar) that cannot be removed with a toothbrush. Your dentist or periodontist will identify these tartar deposits during your regular dental inspection and remove them as part of a professional clean. After the deposits are removed, the teeth are polished with special pastes and cups to create a smooth surface that is less likely to accumulate plaque.
What Are The Consequences Of Periodontal Disease?
Complications
Periodontal disease may put you at greater risk of a number of serious medical conditions:
Heart Disease And Stroke
Gum disease can increase the risk of heart attack and stroke. Research suggests inflammation caused by periodontal disease may be responsible for the connection. The bacteria responsible for gum disease can travel through bloodstreams to the heart where they initiate inflammation and arterial narrowing that cause heart attacks. Oral bacteria can entice the body develop blood clots that increase the risk of a stroke.
Complications Of Pregnancy
Pregnant women with moderate to severe gum disease are more likely to give birth prematurely in comparison with women with healthy gums. Although the connection is inconclusive, having gum disease appears to limit the growth of the fetus and trigger the production of the substances that initiate labour. This is more apparent in cases of severe gum disease that gets worse during pregnancy. The problem gets increasingly worse for women with diabetes and who are already considered a high risk of pregnancy problems.
Uncontrolled Blood Sugar
If left uncontrolled, diabetes puts the whole body at risk of developing complications. By developing periodontal disease and other infections, the body’s ability to use insulin is affected, making blood sugar level harder to control.
Pneumonia
If you have gum disease and lung problems, the travelling bacteria from your mouth to your lungs may cause aspiration pneumonia, a condition that is common in hospitals where patients are sedated or have tracheal tubes.
What Are The Risk Factors For Periodontitis?
Periodontal disease is an infection of the tissues that support the teeth. It begins with plaque: an invisible, sticky film formed on the teeth when starch and sugar in food interacts with bacteria in the mouth. It usuually gets removed by brushing.
Plaque that stays on the teeth longer than 2-3 days can become tartar which can only be removed by professional cleaning. Tartar can damage part of the gum around the base of the teeth and cause gingivitis, the mildest form of periodontal disease. If the issue not addressed early, gingivitis may lead to more serious, destructive forms of periodontal disease called periodontitis.
The inflammation develops pockets between the gums and teeth that fills with plaque and bacteria. Over time, the pockets gradually deepen and progress further under the gum line. The deep infection causes damage to the integrity of the gum tissue and eventually leads to the loss of teeth.
Hygiene
Although the cycle normally starts with poor maintenance and hygiene there are other factors that contribute to the condition:
Hereditary
There is a hereditary element to periodontal disease. If you are doing everything to maintain a good oral health and still suffer from gum disease you might have inherited a pre-disposition to periodontal problems.
Drugs
Oral application of drugs such as cold medicine, oral contraceptives and antidepressants suppress the production of saliva (which has a cleansing effect). The lack of saliva production causes plaque and tartar build up. Drugs such as anti epileptics, especially phonation (Dilantin) and immune suppressants are among the medicines that can cause gingival overgrowth.
Hormonal Changes
Changes in hormones during pregnancy can make the gums prone to disease.
Smoking /Tobacco Use
Tobacco use in any form has significant contribution to periodontal disease. Tobacco damages the immune system, putting the gums at greater risk of infection. Research shows even passive smoking contributes to gum disease. The normal signs of gum disease (bleeding and swollen gums) are usually not prevelent in smokers and are less likely to respond to treatments.
Diabetes
Diabetic people are more likely to develop gum disease due to infection susceptibility. Gum disease is considered one of the complications of diabetes. Diabetes thickens the blood vessels, which carry oxygen and nutrition to body tissues and remove waste. The thickening of the blood vessels slows down the flow of blood and delivery of nutrition and removal of waste. This gradually damages the gums and increases the risk of infection.
Diet
Poor diet can damage body’s immune system and impair the body’s capability to fight infection. For example: low levels of vitamin C and Calcium has been found to contribute to periodontal disease as Calcium strengthens the bone that supports teeth while Vitamin C maintains the integrity of supporting tissues.
Stress
Stress has been linked to many health conditions such as cancer and hypertension. Research has shown that stress can contribute to periodontal disease by making it difficult for the body to fight infections.
How Is Periodontitis Treated?
With careful assessment and treatment, it is possible to halt the progress of periodontitis. The key to success is to eliminate the bacterial plaque that triggers the disease and establish excellent oral hygiene practices. The steps to halting periodontitis can be summarised as:
Oral Hygiene Instruction And Advice
The aim of the oral hygiene phase of treatment is to reduce the number of bacteria in the mouth and therefore reduce the level of inflammation. Your dental practitioner will first explain the causes of your periodontitis and explain exactly how to keep your teeth and gums clean. You will then be given individual advice on how to use the various cleaning aids most effectively; for example, the most appropriate tooth brushing technique, the correct use of dental floss and interdental brushes.
Professional Cleaning
All soft deposits will be removed from accessible areas of the teeth and the teeth polished and treated with fluoride. Depending on the improvement seen in plaque control and gum health, further instruction and cleaning may be carried out in subsequent visits. The next step would be for your practitioner to remove all bacterial deposits and tartar from the root surfaces and gingival pockets.
Antibiotic Therapy
In some cases, with or without microbiological evaluation, antibiotics are prescribed to deal with active or persistent gum infections, which have not responded to other oral hygiene measures.
Reassessment
After several weeks, your dentist or periodontist will make a full assessment of your gums to check the progress of your treatment. A special instrument called a periodontal probe is used to record the depth of any periodontal pockets and check for bleeding from the gums. If periodontal pockets are still present, further treatment options may be suggested, including surgical corrective therapy
Corrective (Surgical) Treatment
Sometimes, a surgical procedure is carried out to clean away plaque bacteria and deposits that are under the gum within periodontal pockets and on the root surfaces at the furcation’s (where the roots diverge). These areas are inaccessible to brushes and floss and inflammation will persist in these sites if bacteria are permitted to colonise them. Under local anaesthesia, the gum is lifted, exposing the root surfaces to be cleaned under direct vision and ensure that all bacteria are removed. Sometimes, it is possible to treat bone loss at the same time using a special regenerative treatment. At the end of the procedure, the gums are sutured back into place around the teeth.
Aftercare – Supportive Periodontal Therapy
The long-term success of periodontal treatment depends both on your own efforts with oral hygiene and those of the practice team who provide your on-going care and assessment. After the first phase of treatment has been completed, your dentist will need to review the condition of your gums at regular intervals to check that the inflammation has been halted. The frequency of your follow-up appointments will depend on the severity of the disease and your individual risk of disease progression. Usually, follow-up visits are scheduled for every three to six months.
Regular follow-up appointments are vital to ensure that the disease process does not recur, causing further destruction of the gums and supporting bone. If there are signs of continuing disease, your dentist will be able to identify new or recurring sites of inflammation and treat them at an early stage. You will also be given advice on how to modify your oral hygiene practices to tackle the inflammation.
Successful periodontal treatment requires your full co-operation in your daily oral hygiene practices and attendance at regular follow-up appointments.
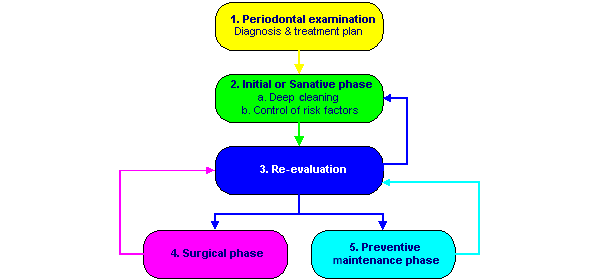
Please Read The Detail Description Of The Periodontal Examination And Treatment Procedure Step By Step:
Periodontal Treatment Overview
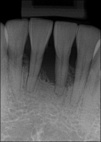
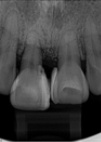
Following the initial examination and radiographs, the goals of the periodontal treatments are to control the cause (bacterial plaque) and the risk factors, repair the damage present (pockets), and restore and maintain a healthy environment.
In order to attain these objectives, there are 5 main steps:
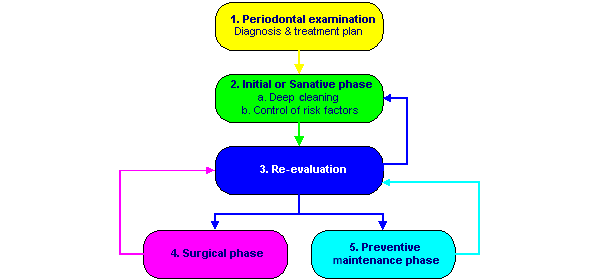
Periodontal Disease Examination
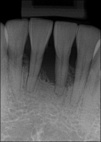
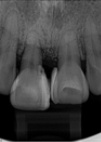
To perform a periodontal disease examination the dentist utilises a metal probe to measure the depth of the gingival sulcus (the gap between your gums and your teeth). The probe is inserted under the gum line at several points in the mouth.
If the gum is healthy the depth of the gum is expected to be 2-3 millimetres. A depth beyond 3 millimetres indicates that a pocket has formed between your gums and your teeth which is a sign of periodontal disease.
 Deep Cleaning:
Deep Cleaning:
This first step is to reduce the gingival inflammation and thus allow the supporting bone to partially recover. For an optimal result, the oral hygiene must be excellent. This step includes the following:
- Personalized oral hygiene instructions using techniques and tools adapted to your needs.
- Scaling and root planing (deep cleaning) to remove the plaque and tartar buildup which adheres to the root surface below the gum line. This procedure is not a surgery, but rather a thorough cleaning (compared to the habitual more superficial cleanings). It is done mainly under local anaesthesia (freezing) and usually requires 2 to 4 appointments.

Special instruments are used below the gum line to remove soft and hard deposits from the tooth surface.

The irritants have been removed from the root surface. Deep cleaning does not eliminate deep pockets and may have to be redone periodically.
Once the freezing has worn off, there is usually no pain. However some patients may experience the following side effects :
- Tooth sensitivity (especially to cold, although temporary, it may last up to 2 months)
- Contraction of the healing gums (as the inflammation decreases). This may create some spaces between certain teeth.
However, the benefits of the treatment significantly outweigh the potential side effects, especially considering that without the treatment, the teeth would be eventually lost.
Periodontal Re-Evaluation
Periodontal re-evaluation must be done between 6 and 12 weeks after the sanative phase is completed. Your periodontist will re-examine your gums to evaluate the healing that has occurred and determine if additional treatment is needed later.
Treatment may consist of corrective periodontal surgery, non-surgical treatment and preventive maintenance visits. This important phase confirms the short-term improvement in your periodontal condition and determines the long-term potential that can be obtained with further treatment.
Periodontal Surgery
Periodontal surgery will be recommended if it is likely to improve the long term stability of gum condition.
The objectives of the surgical phase are:
- Removal of the plaque and tartar buildup (surgical techniques allow better access to deep tartar deposits)
- Correction of the gingival and bone deformities
- Reduction or elimination of the residual pockets to allow proper access for an efficient daily home-care regimen
- To regenerate the supporting bone if possible
Two Surgical Approaches Are Possible:
1. Resective Treatment:
Consists of reducing the pocket depth by reducing the thickness of the gingiva (gums).

Before the surgical phase

After resective surgical treatment
2. Regenerative Treatment:
It consists in regenerating (rebuilding) the bony support and gum attachment to the tooth root. Although this technique is preferable to the resective approach, it requires several prerequisites that are seldom present. Furthermore, its outcome is less predictable.

After resective surgical treatment

At the time of surgery, various materials can be placed in the bone defect to enhance or promote bone regeneration.

Ideal goal of the regenerative surgical treatment. (Due to limitations in current materials and variations in local and host factors, complete regeneration is seldom achieved.)
Although the benefits of surgical treatment outweigh the side effects, these may include:
- Gingival recession (longer teeth)
- Spaces between teeth secondary to the bone loss
- Aesthetic change and increased cold sensitivity, which is usually of short duration.
Periodontal Treatment Maintenance
The periodontal treatment maintenance phase is of utmost important. In order to maintain the high level of periodontal health obtained with the treatment rendered thus far, it is crucial to meticulously follow the recommended home-care instructions daily.
Depending on your specific needs a maintenance recall frequency will be recommended. Preventive maintenance appointments allow us to determine the stability of your periodontal health and intercept any minor problems before they become major ones.
When treated and maintained properly, long-lasting and predictable results are expected.
Risk Factors:
Several risk factors, although incapable of starting periodontal disease on their own, can speed up its evolution and render it unstable when in the presence of inflammation.
In an effort to eliminate these factors, some of the following treatments may be required :
- Making of a bite plane to control the trauma caused by teeth grinding (bruxism)
- Occlusal adjustment
- Splinting of weakened adjacent teeth
- Extraction of untreatable teeth
- Antibiotics
- Smoking cessation
Is Your Gum Healthy?
Check the health of your gums by asking yourself the following questions:
- Are your gums swollen? (Compare the appearance of your gums with those in the picture of healthy gums on the right)
- Do your gums bleed when you are brushing, use a toothpick or other cleaning device?
- Have your gums shrunk back or receded, so that your teeth appear lengthened?
- Are you aware of any loosening of your teeth?
- Do you see any yellowish, pus-like fluid at the gum line when you massage your gums?
- Have your teeth drifted or changed position, have any gaps appeared between them?
- Have your parents or siblings lost teeth prematurely due to tooth loosening?
If you have answered one or more of these questions with ‘yes’, you should contact your dental practice for a periodontal assessment.
Don’t forget that regular check-up appointments with your dentist (at least twice yearly) will enable your dentist to check your periodontal health – ask for the periodontal screening index.
Other Conditions
Are You Diabetic And More Than 40 Years Old?
If the answer is yes, please read the important information below, this relates to your dental health.
Diabetes mellitus is a condition in which the body is unable to control its sugar levels properly. It is an increasingly common disease in western countries, affecting at least 5% of the population. In fact, it is thought likely that only about half of people affected with diabetes have been diagnosed with the disease. Overall, 80% of known diabetics are more than 40 years of age, with just 0.05% below the age of 15 years.
Dentists now know that, in patients with diabetes, untreated periodontal disease progresses rapidly, often leading to early tooth loss. In addition, wound healing following dental extractions is often slow and inefficient. Other problems that might be encountered are abscesses (painful infections), gingivitis with ulcers or sores, and fissures or cracks at the corners of the mouth. Anti-diabetic medications may also cause a patient to suffer from a very dry mouth, which makes dental decay more likely.
Diabetes And Periodontal Disease
Patients with Type 1 (primary, insulin-dependent) diabetes and the more common Type 2 (non-insulin dependent) diabetes each have a three times greater risk of periodontitis, compared with non-diabetic individuals. There is also a higher chance that they will suffer bone loss and experience an aggressive form of the disease. In turn, the presence of unrecognised or untreated periodontitis makes it more likely that their diabetes will be poorly controlled. Therefore, treatment of periodontal disease in diabetic patients is crucial, not only to preserve the teeth, but to help prevent possible complications of uncontrolled diabetes.
It is important – and heartening – to realise that a patient with well-controlled diabetes has no greater risk of periodontal disease than a non-diabetic person. Therefore, it is very important to make sure that blood sugar levels are under control when combating periodontal disease – the better the diabetic control, the more successful periodontal treatment will be.
See below measures can you take to help yourself? [Link]
Kidney Disease And Dialysis
One potential complication of diabetes mellitus, especially when poorly controlled, is irreversible damage to the kidneys. This damage may progress over time until kidney function is severely impaired and either dialysis or a kidney transplant is necessary.
It is very important for the overall health of patients with kidney disease that their mouth should be free from inflammation and bacterial build-up. However, oral hygiene can be a low priority for dialysis patients, because of the demands of their treatment for kidney disease, with the result that periodontal disease and tooth decay are commonly seen. This is an added disease burden for the body and is likely to weaken its ability to cope with the systemic disease. Excellent oral hygiene and treatment of all decayed teeth is essential.
See below measures can you take to help yourself? [Link]
Organ Transplant Recipients And The Risk Of Periodontitis
Before an organ transplant is carried out, the mouth should be free of periodontal disease and dental decay. Therefore, it is important to arrange to be examined by your dentist prior to the operation, so that decisions can be made about any necessary treatment, in conjunction with your transplant specialist.
After the transplant procedure, you will need to take long-term immunosuppressive therapy in order to prevent organ rejection which will increase your risk of periodontal disease. One of the most commonly used immunosuppressive drugs is called cyclosporine A. Medications to lower blood pressure, such as calcium antagonists, are also often prescribed to transplant recipients. In many people, these medications cause a thickening of the gums, known as gingival hyperplasia, after a few months of treatment and this outcome is known to be more likely if inflammation is already present in the gums. The gum enlargement develops mainly between the teeth, appearing as small swellings, but it may develop into more generalised bulging of the gums. The overgrown gums partially cover the teeth and make plaque removal very difficult, leading to the onset of inflammation.
See below measures can you take to help yourself? [Link]
Phenytoin Use In Epilepsy
If you take phenytoin to control your epilepsy, your medication could put you at risk of periodontal disease.
Phenytoin is an anticonvulsant drug, which is sometimes used in the treatment of epilepsy. In some people, it causes an overgrowth of the gums which makes cleaning of the teeth very difficult. As a result, bacterial plaque accumulates and triggers inflammatory changes in the gums, leading to gingivitis and, potentially, periodontitis. The enlargement of the gums is more likely to happen if the patient’s oral hygiene is poor or if there are already inflammatory changes present in the gums when treatment is started.
What Measures Can You Take To Help Yourself?
Personal Care At Home
Your cooperation with the oral hygiene recommendations of your dentist is vital to the success of preventive treatment. It is essential that you maintain a regular and thorough cleaning routine at home, including careful tooth brushing twice daily and interdental cleansing once daily. Fluoride toothpastes, mouthwashes and gels will help provide protection against tooth decay.
Professional Care
Your dentist will be able to provide personalised preventive care to care for your gums, including regular professional tooth cleaning, medical treatments and advice. It is advisable to have your teeth professionally cleaned at least twice a year; at these visits, all soft and hard deposits are removed by a specially trained professional (a dentist or hygienist) and your oral hygiene practices are reviewed and if necessary, adjusted. It is very important to attend regular follow-up appointments, so that your condition can be closely monitored.
If a combination of oral hygiene measures and professional cleaning is not enough to reduce or limit the gum overgrowth to a manageable level, your dental practitioner might suggest that you have surgery to trim and reshape the gum, to improve the appearance, function and access for home care. Your dentist will liaise with your physician to make sure that you have the correct antibiotic and steroid cover for this procedure.
Clinical Crown Lengthening
Clinical crown lengthening procedure is required when the tooth is fractured or has very large filling to restore the tooth to normal function.
Clinical crown lengthening procedure involves the removal and re-contouring of the gum and bone surrounding the tooth. This provides your dentist with a sufficient amount of tooth to work with. The crown is placed so it will remain on the tooth and allow for healthy gum tissues.

Example of a healthy tooth.

Example of a tooth fracture below the gum line, into the jaw bone. The restorative dentist cannot access the remaining tooth structure and restore this tooth adequately.

A periodontal procedure is required to remove some bone and expose the remaining tooth structure.

Final bone and gum level after healing. The remaining tooth structure is accessible to the restorative dentist.

The tooth is restored with a filling. Depending on the remaining tooth structure, a crown may also be required to restore the tooth.
Why Do Gums Recede?
To understand why gums recede it is important to know the anatomy of the tooth and its supporting structures.

A healthy tooth is surrounded by two types of gum tissue. The attached tissue (1), a leather-like solid tissue bound to the jaw and tooth. A minimum amount of attached tissue is crucial for the stability of your gums. A loose fragile tissue, called mucosa (2), which is not bound to the tooth or the jaw.

When the attached tissue is very thin (1), the area becomes more susceptible to breakdown. Brushing too hard in this area may sometimes speed up the breakdown.
Gum tissue breakdown, called recession, results in exposure of the root surface. This process can be progressive and gradually expose more root surface. Severe recessions can jeopardise the long-term survival of the tooth.

The recessions can create areas that are difficult to clean. If the areas are not brushed properly, plaque deposits will cause gingivitis. Gingivitis can speed up the breakdown in the area. These areas can also be more sensitive to cold.
Untreated progressive recessions can lead to tooth loss.
Gum Graft
A gum graft (also called free gingival graft) increases the attached tissue and stops the progression of recessions. It is placed at the base of the tooth and does not cover the already exposed root surface. The success rate of this procedure is excellent and its benefits should last a lifetime. Healing can be compromised with smokers.

A graft is a thin piece of gum tissue usually taken from the roof of the mouth. Its main purpose is to stop the progression of the recession.

The graft is usually placed at the base of the recession, to strengthen the attached tissue and prevent further recession.

This is a picture showing some recession and thin attached tissue.

This is the same tooth after a graft successfully increased the attached tissue.
 Out of hours emergency:
Out of hours emergency:
 148 Ewell Road, Surbiton, Surrey, KT6 6HE
148 Ewell Road, Surbiton, Surrey, KT6 6HE


 0208 33 99 333
0208 33 99 333













 Deep Cleaning:
Deep Cleaning: